Florida’s providers are buzzing with questions about value based care, asking why now? Is it a fad? Will it really ever be a widespread form of payment? Why does Florida seem farther behind the value based curve than other markets?
While there are more aggressive markets in other parts of the country, the bottom line is this: CMS changes are coming and they will not be stopped. The government has invested too much money to turn around at this point. Here are just a few examples of why:
- The CMS Value Based Program with hospitals is already implemented;
- Center for Medicare and Medicaid Innovation is piloting NUMEROUS programs covering many physician specialties
- CMS expanded the Medicare Shared Savings Program to 3 tracks.
- A new Merit-Based Incentive Payment for Physicians, Physician Assistants, Nurse Practitioners, Clinical Nurse Specialists, and Certified Registered Nurse Anesthetists will be apply to payments for services furnished in 2019.
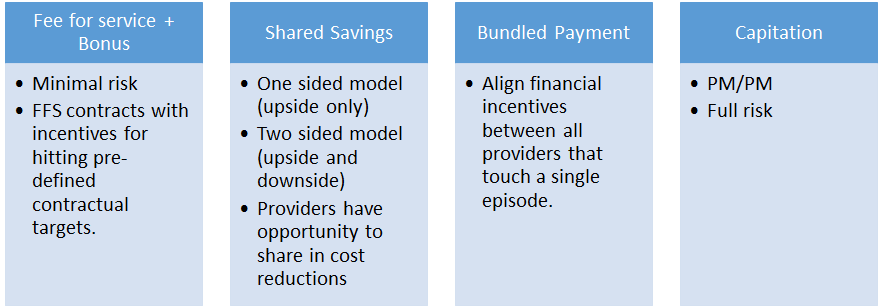
The train has left the station. Providers will now shift from fee for service to value based payments with CMS. To be successful and still have a profitable business, clinical integration and quality improvements will need to be implemented to improve your practice whether you are hospital based or office based AND whether you are employed by a hospital or in private practice. These changes will be implemented for all of your patients as you will not distinguish in your level of service between patients with managed care as the payor rather than CMS. This essentially means that managed care payors will reap the benefits of these improvements in your practice. If you do not have a value based contract in place with the managed care payors they will not be sharing one dime with you. They will reap the benefits of your improvements AND keep the money! And by the time you get around to a managed care contract that is value based, the shared savings opportunities will be less than if you began those discussions now. Continue reading